La implementació d’un cribratge amb el factor de creixement placentari (PIGF), una proteïna que promou el creixement dels vasos sanguinis i de la placenta i que en gestacions amb risc de preeclàmpsia està disminuïda des del primer trimestre de la gestació, en un entorn d’assistència clínica de forma contingent, identifica un alt percentatge de casos que tenen risc de desenvolupar preeclàmpsia (80%). En aquests casos, el tractament amb aspirina a baixes dosis entre les 12 i les 36 setmanes ha reduït, en el nostre medi, en un 68,4% el desenvolupament de preeclàmpsia (PE) preterme.
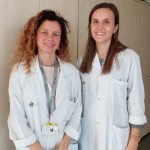
És la principal conclusió de l’estudi fet a Sant Pau1 i que, segons la Dra. Elisa Llurba, directora del Servei de Ginecologia i Obstetrícia i cap del Grup de Medicina Perinatal i de la Dona de l’Institut de Recerca de l’Hospital de la Santa Creu i Sant Pau, “en l’actualitat el cribratge de preeclàmpsia es realitza amb criteris d’història clínica materna (per exemple, haver patit una PE anteriorment), més la pressió arterial i l’avaluació del flux a les artèries uterines a l’ecografia de les 12 setmanes. Aquest cribratge, si bé és capaç d’identificar un 65-70% de les dones que desenvoluparan preeclàmpsia preterme, es pot millorar amb l’ús del PlGF. Tot i això, l’ús d’aquest biomarcador no es contempla dins del sistema sanitari pel seu cost. En el nostre estudi hem demostrat que només fent ús aquest biomarcador en un grup reduït de pacients amb un risc intermedi de patir la malaltia, hem obtingut uns resultats semblants als protocols que utilitzen el PIGF en tota la població, amb l’estalvi corresponent per al sistema sanitari i, per tant, fent-lo sostenible i implementable a curt termini”.
La Dra. Cristina Trilla, primera signant de l’estudi, afegeix que “els biomarcadors ofereixen un potencial per al diagnòstic precoç, abans que apareguin els símptomes clínics, però avui encara no disposem de dades procedents de l’assistència clínica i calen més evidències científiques. Però, precisament, un dels punts forts de l’estudi és que s’ha dut a terme en la pràctica clínica actual del Servei de Ginecologia i Obstetrícia de Sant Pau”.
La preeclàmpsia és una malaltia específica de l’embaràs, multifactorial i d’afectació multisistèmica (sobretot, ronyó, fetge i cervell), definida com a una hipertensió que apareix a partir de les 20 setmanes de gestació2. Avui, cal fer proves de detecció a totes les embarassades i el cribratge del primer trimestre de la preeclàmpsia prematura s’inclou en el Protocol de Seguiment de l’Embaràs3 a Catalunya des del 2018. Segons aquest document, cal combinar factors materns i obstètrics, com la pressió arterial mitjana (PAM), el Doppler de l’artèria uterina (UTPI) i la proteïna A plasmàtica associada a l’embaràs (PAPP-A) -i cal oferir àcid acetilsalicílic a les dones embarassades amb alt risc fins a la setmana 36 de gestació.
Però la preeclàmpsia no es pot predir només pels antecedents obstètrics i/o la presència de factors de risc clínics. En aquest sentit, en els darrers anys s’han proposat molts biomarcadors de detecció en el primer i segon trimestres, que sols o combinats amb altres paràmetres permeten identificar pacients amb risc de preeclàmpsia i predir la seva evolució. Però aplicar un protocol de cribratge universal amb models multivariants, com el PIGF, és tot un repte.
L’estudi del Servei de Ginecologia i Obstetrícia de Sant Pau – IIB Sant Pau, fet en col·laboració amb el Servei de Bioquímica del mateix centre i la Facultat de Medicina de la Universitat Autònoma de Barcelona, s’ha dut a terme en dues fases incloent-hi 1.372 dones embarassades abans de fer l’ecografia del primer trimestre, definint tres grups de risc: alt sense proves addicionals, mitjà que requereix proves addicionals, i baix risc.
En la primera fase, es va dur a terme un protocol prospectiu de cribratge en una cohort històrica de 525 dones amb embarassos únics entre el juliol del 2016 i el novembre del 2018, aplicant els factors materns (ètnia, pes, talla, tabaquisme, antecedents de preeclàmpsia, diabetis preexistent, hipertensió, trombofília, afeccions renals o autoimmunes), els marcadors biofísics (pressió arterial mitjana i Doppler de l’artèria uterina) i la proteïna A plasmàtica associada a l’embaràs (PAPP-A), obtenint un risc preliminar de preeclàmpsia. El PIGF també es va afegir en el model predictiu, concretament en les pacients amb risc mitjà de preeclàmpsia.
En aquesta fase, un 11,4% de les dones (60) presentaven un risc alt de preeclàmpsia i un 21,5% (113) tenien un risc mitjà. En 102 d’elles es va afegir el PlGF. L’índex final de les embarassades amb un alt risc va ser del 17,3% (91) i la xifra final de casos de preeclàmpsia va ser del 4% (21). D’ells, en el 47,6% (10) la preeclàmpsia va ser prematura i en el 52,4% (11) va ser tardana.
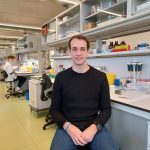
La segona fase de l’estudi de Sant Pau va consistir en un treball prospectiu de base poblacional entre l’1 de febrer del 2019 i el 28 de febrer del 2020 dut a terme en 874 dones. En la primera etapa del cribratge, un 8,7% de les dones (74) tenien un alt risc de preeclàmpsia i un 15,3% (130) requerien un segon cribratge amb PIGF. L’índex final de positius en preeclàmpsia va ser del 14,9%. La incidència de preeclàmpsia prematura (menys de 37 setmanes) es va reduir significativament, en un 68,4%, després d’haver aplicat el nou model de cribratge.
Segons la Dra. Llurba, “després d’un any de cribratge prospectiu, determinant el PlGF en el 15% de la nostra població, hi ha hagut una reducció significativa (del 68%) de la preeclàmpsia preterme i, de fet, pràcticament ha desaparegut la preeclàmpsia abans de les 34 setmanes, que era la que més condiciona la mortalitat materna i neonatal”. Afirma que, “la mostra inclosa en el nostre estudi és limitada, però la reducció de la incidència de la preeclàmpsia preterme va ser coherent amb investigacions anteriors i aplicar el cribratge amb PIGF en la pràctica clínica és factible amb protocols ben definits”.
Referències bibliogràfiques
1. Reduction in Preterm Preeclampsia after Contingent First-Trimester Screening and Aspirin Prophylaxis in a Routine Care Setting. Diagnostics 2022, 12(8),1814;
https://doi.org/10.3390/diagnostics12081814. Cristina Trilla, Josefina Mora, Nuria Ginjaume, Madalina Nicoleta Nan, Obdulia Alejos, Carla Domínguez, Carmen Vega, Yessenia Godínez, Monica Cruz-Lemini, Juan Parra, Elisa Llurba
2. Obstetrícia i Ginecologia. Revista oficial de la Societat Espanyola de Ginecologia i Obstetrícia (SEGO). Guia d’Assistència Pràctica. Trastorns hipertensius en la gestació
3. Protocol de Seguiment de l’Embaràs a Catalunya. Departament de Salut de la Generalitat de Catalunya