Experts agree that today we are much closer to defeating Alzheimer’s and that we are living through a historic paradigm shift. There is still no cure, but for the first time it has been possible to slow the course of the disease thanks to a turning point: a new generation of drugs that remove the beta-amyloid protein that accumulates in patients’ brains and slow the progression of Alzheimer’s by 30%. Plasma biomarkers are also highlighted as a revolution in diagnosis at all stages of the disease through a simple blood test. They also deliver a public health message to society: 45% of dementia cases could be prevented or delayed by addressing 14 modifiable risk factors. These are some key conclusions from the recent meeting marking the 20th anniversary of the Memory Unit (MU) at Hospital de Sant Pau, which brought together world experts, patients, and families.
“We have very robust biomarkers that enable highly accurate diagnosis, drugs that modify disease progression, and 130 additional medications currently under study that broaden the range of strategies, including approaches focused on inflammation and synaptic protection… Every day we can and must open another door in the fight against Alzheimer’s, and I am convinced that we will ultimately defeat this neurodegenerative disease,” emphasized the renowned neurologist Teresa Gómez-Isla, Chief of the Memory Disorders Division at Mass General Brigham (Massachusetts General Hospital) and Professor of Neurology at Harvard Medical School (U.S.), who was also part of Sant Pau’s MU in its early years.
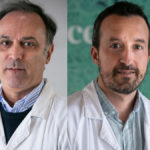
“In 2026, the 21st century begins in Alzheimer’s,” stated Dr. Juan Fortea, current director of the MU. “These new drugs represent a radical change and are only the first step toward a future we have every reason to view with great optimism.” Dr. Alberto Lleó, Director of the Neurology Department at Sant Pau, noted that “we will see many treatments coexisting.” He added that these changes “pose a major challenge: a new model of patient management requiring much closer monitoring. New infrastructure, personnel, and technology are needed.” He also stressed that Sant Pau “is very well positioned to continue being a global leader in this field.”
Dr. Adrià Comella, Director of Hospital de Sant Pau, stated at the opening of the event that “our center is a leader and pioneer in this field, always working from a systems perspective and through contributions and collaborations with other institutions. The Memory Unit is a clear example.” Meanwhile, Dr. Jordi Surrallés, Director of IR Sant Pau, highlighted “our global leadership in Alzheimer’s research and in the genetic forms of this disease, and we are carrying out intensive work in the identification of biomarkers.”
A Decisive Advance: Plasma Biomarkers
Dr. Gómez-Isla, with an extensive clinical, research, and teaching career—who treated former Barcelona mayor Pasqual Maragall—studies brain changes associated with aging, particularly in the earliest stages of Alzheimer’s, mechanisms of brain resilience, and the validation of new imaging biomarkers for early detection and intervention. She addressed these topics in “Alzheimer’s: Deciding the Future of Memory” and stated that “with the MU came a conviction: science must go hand in hand with patient care,” recalling the beginnings of a career defined by translational research.
“Imaging and plasma biomarkers have been a key breakthrough. Previously, definitive diagnosis was only possible through postmortem brain analysis. Now we have tools that allow us to identify the disease during life, such as the plasma biomarker p-tau217, which has demonstrated a strong ability to distinguish Alzheimer’s from other neurodegenerative diseases, even outperforming other blood and MRI biomarkers. These simple, noninvasive methods open the door to reliable and more accessible detection.”
Another advance is the recently approved drugs. At Massachusetts General Hospital, data from the first two years of treatment have been analyzed: “We need to see how the benefits observed in clinical trials translate into patients’ daily lives, but these advances are a ray of hope for patients and families.” She added that “measuring benefits in each patient is not easy, because each individual is different and comorbidities make it difficult to understand how Alzheimer’s progresses and to assess the effectiveness of these treatments.”
She also reviewed important milestones in Alzheimer’s research, such as genetic evidence. “It was known that 90% of Alzheimer’s cases occurred in people over sixty years of age, while 10% affected younger patients, often due to genetic causes. This evidence was crucial in formulating the amyloid cascade hypothesis: first, beta-amyloid accumulates abnormally, then the tau protein, and finally progressive loss of neurons and synapses occurs, leading to clinical symptoms.”
She also highlighted a pioneering 1996 study demonstrating marked neuronal loss in the entorrinal cortex—key for memory and recollection—from very early disease stages, disproving the belief that aging inevitably entailed generalized neuronal loss. “A healthy human brain has about 7 million neurons in this region. In patients with very mild Alzheimer’s symptoms, a 30% neuronal death rate was observed, which could reach 70% in advanced stages. This indicated that brain damage began many years before the first symptoms and underscored the need for earlier and better diagnosis.” Today we know that brain amyloid can begin to be detected up to fifteen years before symptom onset in certain cases, defining a long silent phase that represents the best therapeutic window before neuronal loss becomes irreversible.
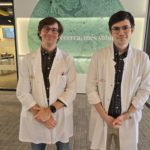
Sant Pau and the Memory Unit, A Global Reference in Alzheimer’s
Hospital de Sant Pau created Spain’s first Neurology Department in 1882. Since then, it has remained a pioneer in this field in both clinical care and research. In 2005, it created the MU with four members: Dr. Rafael Blesa, Dr. Alberto Lleó, Dr. Isabel Sala, and Dr. Gómez-Isla; today, it is an interdisciplinary team of 75 professionals. “Additionally, Dr. Isabel Illa was instrumental in promoting research and establishing the laboratory during the early years,” said Dr. Lleó.
Today, Sant Pau holds a key position on the global Alzheimer’s landscape, and the MU has recently been designated a CSUR (National Reference Center) for rare diseases in adults presenting with cognitive disorders. It is the world’s leading recruiting center for clinical trials in this disease, notably through the SPIN Cohort (Sant Pau Initiative on Neurodegeneration), which is essential for biomarker discovery and validation, and the DABNI Project (Down Alzheimer Barcelona Neuroimaging Initiative), an intensive biomarker study in adults with Down syndrome (DS) and Alzheimer’s. “We have conducted more than 1,000 clinical visits with DS patients with Alzheimer’s, making it by far the largest biomarker cohort in DS worldwide,” explained Dr. Fortea. “We have reconceptualized DS, and in 2024 it was incorporated into U.S. diagnostic criteria.”
All of this has made the center a benchmark for collaboration. Clear examples include the HUB Alzheimer Barcelona, bringing together six reference centers in Barcelona; the Global Brain Health Institute (GBHI), coordinated by the University of California (U.S.) and Trinity College Dublin to promote a global network of brain health leaders; and Brave-AD (Barcelona REsearch on APOE, Vascular Risk and Eye in Alzheimer’s Disease), among others.
Currently, the MU is conducting 28 clinical trials involving the main molecules related to Alzheimer’s and is a reference center in biomarkers. Notably, it has identified a new genetic form of Alzheimer’s: specifically, having two copies of the APOE4 gene causes the disease in 95% of cases—previously considered only a risk factor, it is now known that virtually all individuals with this duplication will develop the disease. Between 2% and 3% of the population and 1 in 5 people with dementia carry this duplicated gene. “Being able to predict who will develop the disease can be extremely useful to begin treatment before the first symptoms appear,” stated Dr. Fortea regarding the study published in Nature Medicine.
Another study published in JAMA Neurology reinforces the role of blood testing in the future of dementia diagnosis and monitoring, demonstrating that the plasma biomarker p-tau217 achieves 90–95% accuracy, comparable to cerebrospinal fluid biomarkers, even in the earliest stages of the disease when symptoms are not yet evident.
Keynote Lecture by Dr. Rafael Blesa, Founder of the MU
Under the title “Four Decades of Research in Alzheimer’s Disease and the Development of Memory Units in Catalonia”, Dr. Rafael Blesa, an internationally recognized neurologist in Alzheimer’s research and study, founder of the Sant Pau MU and former Director of the Neurology Department at Sant Pau, reviewed the most important milestones in recent Alzheimer’s history, including studies on the genetics of the disease, the amyloid cascade hypothesis, approval of the first drugs to treat symptoms, the creation of family associations, pioneering programs such as PICOGEN, diagnostic protocols, advances in neuroimaging and biomarkers, and the establishment of memory units in Catalan hospitals.
Looking ahead, he stated that “there will be more than symptomatic treatment with the newly approved drugs” and that “we must continue investigating the cause of the disease, because none of the current therapies can cure it.” He also emphasized “interdisciplinary care aligned with social policies, frameworks such as PLADEMCAT that guide comprehensive care, and public education about modifiable risk factors in the development of Alzheimer’s.”